Coping with the Monkey pox outbreak
The current Monkey pox outbreak has
again exposed Nigerians to the dangers of preventable and treatable diseases.
Lassa fever, Cerebrospinal Meningitis, CSM and Cholera are just a few of the
emergency epidemic outbreaks the country has so far witnessed this year.
 | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Pupils running away from schools over alleged deadly Monkey pox vaccination |
September 22, 2017, the Nigerian
Centre for Disease Control, NCDC, received a report of a suspected Monkey pox
virus disease from the Niger Delta University Teaching Hospital, NDUTH,
Okolobiri, Bayelsa State. In less than a month, the Monkey pox affected 43
people in Akwa Ibom, Cross River, Ekiti, Lagos, Enugu, Nasarawa, Rivers, and
FCT.
For 24 days, the disease carried the
tag of “suspected” until the Federal Government obtained laboratory evidence
from the World Health Organization, WHO, Regional Laboratory in Dakar, Senegal,
to confirm three of the cases in Bayelsa State. The latest outbreak is the
third in Nigeria’s history, with previous episodes in 1971 and 1978 according
to the WHO.
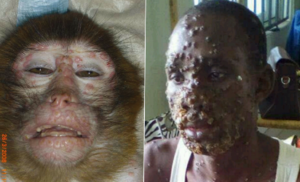
Monkey pox is a rare disease caused
by infection with the Monkey pox virus which belongs to the same family of
viruses that cause small pox. African rodent species are believed to be the
natural reservoirs and play a role in transmission. The virus can cause an
illness with symptoms of a generalized vesicular skin rash, fever and painful
jaw swelling. In previous outbreaks, it led to death in at least one in 10
people.
With no available protective
vaccine, no specific treatment and no cure, there is the need to raise
awareness about the risk factors of monkey pox and employ public education
about the measures that must be taken to reduce exposure to the virus.
Transmission is in two modes – animal to human and human to human. Prevention
of contact with natural hosts of the virus – monkeys, rodents, rats, squirrels
and others, helps break transmission from animal to human. Avoidance of contact
with the body fluids and personal items of infected persons prevents
human-human transmission.
The poor state of our national
health services remains worrisome and the spread, in recent times, of
infectious diseases amplifies the gaps in the nation’s emergency preparedness
plan. The latest outbreak expresses the need to establish and equip public
health laboratories, human vaccine laboratories and integrated surveillance
systems.
It also showcases the need to employ
effective and sustainable approaches in curtailing disease epidemics and calls
for commitment to strengthen the health system to a level of sustainability and
effectiveness.
It is unacceptable that Nigeria lacks the
facilities to diagnose and confirm most infectious outbreaks. Now is the time
to revive and equip the national laboratory facilities to regain the lost glory
that it once had in the quick confirmation of many of these diseases.
pictures below:





Comments
Post a Comment
comment here